IASON is a joint project of Tokeya Deep Data Dive GmbH & Co. KG and the chair of clinical psychology and psychotherapy (KliPs) at the Friedrich-Alexander-University (FAU) Erlangen-Nuremberg.
The name “IASON” means “the healer” in Greek and is a heroic figure from Greek mythology.
On the one hand, the IASON project aims to develop a tool for the simple and rapid early diagnosis of Alzheimer's dementia. This tool will be based in particular on the analysis of data from electroencephalography (EEG) and other characteristic data, which are available in significantly altered form in Alzheimer's dementia.
The second focus of the IASON project is the development of an intelligent, emotional-empathetic digital assistant (IEEDA), which supports patients as well as their relatives and nursing staff in communicating with Alzheimer's patients in a variety of sensitive ways.
The IASON project is funded by the Federal Ministry of Education and Research (BMBF), see project description (BMBF), and was selected by the BMBF for the “Project Gallery 2019” alongside 13 other of the funded projects 2019 in the area of “Human-Technology Interaction”.
Note:
In the times of the COVID-19 crisis, the IASON project must also change. We will also make our contribution to support the dementia patients to be cared for in times of the threat of COVID-19! More about this under “The IASON project in times of the COVID-19 crisis”.
Due to the development of the COVID-19 crisis, we feel compelled to publish this project page currently in a temporary transition stage.
The project will undergo some structural changes due to the necessary measures to protect the patients, which can only be reported on at a later date, e.g. after the summer holidays 2020.
For this reason, the individual points of content, particularly with regard to the project structure, objectives and methods used, are only briefly presented here in a concise form and will be updated in a concrete manner at a later date.
News
Poster presentation at AAIC 21 of Tokeya
Our poster on the transition zone between motor and cognitive function in Long Covid, Parkinson’s and Alzheimer’s disease patients was published at AAIC 21 (26 - 31/07/21) in Denver, Colorado, USA.
A new EEG biomarker, the Frontal Asymmetry Index (FAI), was presented that can be used to clearly distinguish between Alzheimer’s disease patients and control subjects.
Furthermore, first results of 40 Hz neurostimulation in a Long COVID patient suffering from tremor and chronic fatigue syndrome were presented.
The first results justify the statement that sensory neurostimulation at 40 Hz can eliminate the pathological peaks at 20 Hz typical of tremor and Parkinson’s disease. The durability of this effect as well as the transferability to Alzheimer’s disease are currently being investigated.
Files:
- Poster presentation (MP4, 1920×1080 px, 5,2 MB)
- Slides (PDF, 10,8 MB)
- Abstract (PDF, 353 KB)
- Transcript (PDF, 66 KB)
- Questions and answers (PDF, 141 KB)
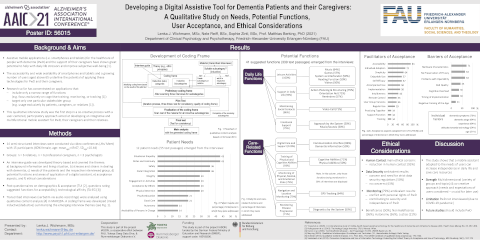
Poster presentation at AAIC 21 of KliPs (FAU)
Also from our partner in the joint project IASON, the Institute of Clinical Psychology (KliPs) at the Friedrich-Alexander-University Erlangen-Nuremberg (FAU), a poster was presented under the title "Developing a Digital Assistive Tool for Dementia Patients and their Caregivers - A Qualitative Study on Needs, Potential Functions, Practical Requirements, User Acceptance, and Ethical Considerations") as part of the IASON collaborative project at AAIC21.
This is the planned preliminary study on user acceptance of a smart digital assistant by dementia patients and their caregivers. This preliminary study was conducted using telephone interviews with caregivers due to corona-related limitations.
Preliminary results showed that dealing with symptoms of dementia in everyday life was burdening. Emotional needs in patients and needs for additional care resources in relatives and caregivers were the most important unanswered needs. 53 functions were suggested in the areas: digital care, support, training, monitoring, navigation, leisure activities, and social contacts. Participants had ethical requirements (i.e. data protection, privacy, and autonomy) that if met, would enhance acceptance. Results on questionnaires showed positive attitudes towards, curiosity about, and no insecurity with regards to technology. The overall acceptability of suggested functions was high.
Files:
Inrease in funding & Announcement of pilot study
We are very pleased to announce that the BMBF has approved an increase of the funding of the company Tokeya Deep Data Dive GmbH & Co. KG for the financing of the IASON project. The new funds will be used to develop an app combining an automated olfactory and memory test, the two positive results of which allow to predict that people will NOT develop Alzheimer's disease with a probability of 96% within the next 4 years (see “Olfactory test” the study of Devanand et al). The olfactory test will also be used to clarify symptoms of COVID-19 odour loss.
Read more ...Loss of sense of smell with COVID-19
The SPIEGEL of 20.8.20 reported on a study on the loss of the sense of smell in COVID-19 diseases, in which the frequency of ACE2 receptors, which are used by the SARS-CoV-2 virus as entry port into the cell, was determined on the basis of human tissue, including the olfactory mucosa.
Read more ...Participation in Conference on Alzheimer’s disease
The partners in the joint project IASON participated in the world’s largest conference on Alzheimer’s disease AAIC, which was originally planned to take place in Amsterdam from 27.7.-31.7.20, but which now had to be conducted virtually due to the COVID-19 pandemic. On 28.7.20 the Swedish research group around H. Zetterberg from the University of Gothenburg reported as a world novelty extraordinary progress in the development of blood tests for the very early diagnosis of Alzheimer’s disease.
Read more ...Sars-CoV-2 and Alzheimer’s dementia
It is now known that people suffering from COVID-19 temporarily lose their sense of smell and taste. This assumes that the viruses invade the olfactory bulb of the brain (Bulbus olfactorius = BO).
Read more ...

 English
English  Deutsch
Deutsch